New York’s governor threatened to fine hospitals if they don’t use their allotment of COVID-19 vaccine fast enough. His South Carolina counterpart warned health care workers they have until Jan. 15 to get a shot or move to the back of the line. California’s governor wants to use dentists to vaccinate people.
With frustration rising over the sluggish rollout of the vaccine, state leaders and other politicians around the U.S. are turning up the pressure, improvising and seeking to bend the rules to get shots in arms more quickly.
Meanwhile, U.S. Health and Human Services Secretary Alex Azar said Wednesday that the government will allow more drugstores to start giving vaccinations to speed delivery. If health workers aren’t lining up fast enough, he said, it is OK to expand eligibility to lower-priority groups.
“We need to not be overly prescriptive in that, especially as we see governors who are leaving vaccines sitting in freezers rather than getting it out into people’s arms,” he said.
As of Wednesday, more than three weeks into the U.S. vaccination campaign, 5.3 million people had gotten their first shot out of 17 million doses distributed, according to the Centers for Disease Control and Prevention. While that is believed to an undercount because of a lag in reporting, health officials are still well behind where they wanted to be.
Across much of the U.S., health care workers and nursing home residents are being given priority for the initial, limited supplies of the vaccine at this stage, but pressure is building to let other groups step up, and some states have given the OK for the elderly to start receiving shots.
The slow rollout has been blamed on a multitude of problems, including a lack of funding and direction from Washington, mismatches between supply and demand, a patchwork of approaches by state and local governments, distrust of the vaccine, and disarray created by the holidays.
The U.S. has an estimated 21 million health care workers and 3 million residents of nursing homes and other long-term care centers. The CDC reported that about 512,000 people in such centers have been vaccinated through a partnership between the government and the CVS and Walgreens drugstore chains.
Azar announced that in addition to the nursing home program, pharmacies from 19 chains will be allowed to help now with dispensing shots to ease pressure on hospitals, which have been the main vaccine providers so far. More than 40,000 drugstores will be eventually be involved, he said.
The pharmacies will still have to follow state guidelines for who gets in line first.
Dr. Anthony Fauci, the nation’s top infectious disease expert, estimated this week that between 70% and 85% of the U.S. population will ultimately need to be vaccinated to achieve “herd immunity,” a goal he said could be achieved by the start of next fall. That translates to as many as 280 million people.
The U.S. death toll, meanwhile, has climbed past 359,000. COVID-19 deaths set another one-day record at 3,775 on Tuesday, though authorities have cautioned that the numbers around holidays can fluctuate dramatically because some health agencies fall behind in reporting cases, then rush to catch up.
With cases and hospitalizations also soaring and a new, more contagious variant of the virus gaining a foothold in the U.S., politicians are getting aggressive in trying to accelerate the vaccination drive. The governors of California, Maryland and North Carolina said they will use the National Guard to speed things up.
Maryland Gov. Larry Hogan warned, too, that any facility that has not administered at least 75% of its first doses may have future allocations reduced until they can speed up vaccinations.
While about 270,000 doses have been put directly in the hands of front-line vaccinators in the state over the last three weeks, Hogan said that only about 77,000 people had been inoculated as of Tuesday, or about 1.3% of the state’s population.
Gov. Henry McMaster of South Carolina warned that health care workers will lose their place in line if they don’t move quickly to get their shots. As of Monday, the state had given out less than half its initial allotment of the Pfizer vaccine to about 43,000 people.
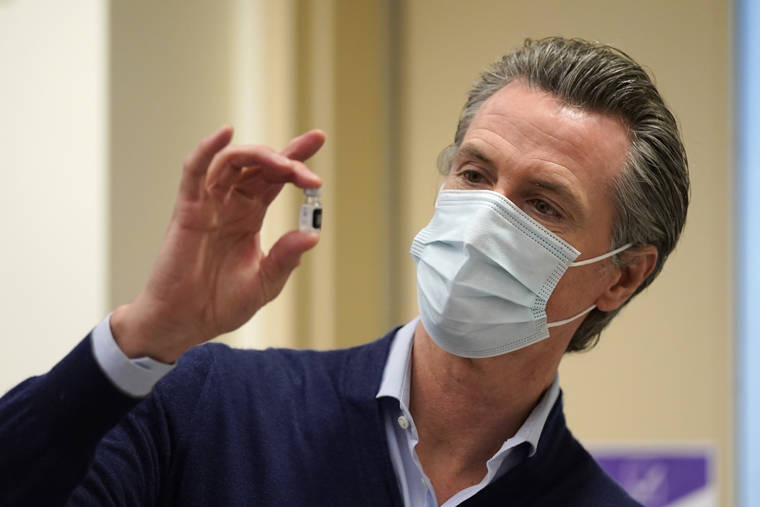
In California, where just 1% of the population has been vaccinated, Gov. Gavin Newsom said he wants to give providers the flexibility to dispense shots to people not on the priority list if doses are in danger of going to waste. He also wants to expand the pool of professionals dispensing shots.
The pace of vaccinations had been so slow in New York that Gov. Andrew Cuomo on Monday threatened to fine hospitals up to $100,000 if they don’t finish their first round of inoculations by the end of the week. He also threatened to stop sending the vaccine to hospitals that don’t use their share promptly.
“Move it quickly. We’re serious,” Cuomo warned. “If you don’t want to be fined, just don’t participate in the program. It’s not a mandatory program.”
The delays prompted New York City Mayor Bill de Blasio to call for eligibility to be expanded, and on Wednesday he announced a plan to provide shots to 10,000 of the city’s police officers by Sunday.
But Cuomo immediately shot down that idea, saying, “We need to get the health care population done first because they are the front line.”
Alaska, meanwhile, announced it is opening the next phase of vaccinations to people 65 and older next week. In Louisiana, people 70 and older are newly eligible this week. And Oklahoma’s most populous county will begin providing vaccinations to residents 65 and above on Thursday.